Management
Diabetes management concentrates on keeping blood sugar levels close to normal, without causing low blood sugar. This can usually be accomplished with dietary changes, exercise, weight loss, and use of appropriate medications (insulin, oral medications).
Learning about the disease and actively participating in the treatment is important, since complications are far less common and less severe in people who have well-managed blood sugar levels. The goal of treatment is an A1C level below 7%. Attention is also paid to other health problems that may accelerate the negative effects of diabetes. These include smoking, high blood pressure, metabolic syndrome obesity, and lack of regular exercise. Specialized footwear is widely used to reduce the risk of diabetic foot ulcers by relieving the pressure on the foot. Foot examination for patients living with diabetes should be done annually which includes sensation testing, foot biomechanics, vascular integrity and foot structure.
Concerning those with severe mental illness, the efficacy of type 2 diabetes self-management interventions is still poorly explored, with insufficient scientific evidence to show whether these interventions have similar results to those observed in the general population.
Lifestyle
People with diabetes can benefit from education about the disease and treatment, dietary changes, and exercise, with the goal of keeping both short-term and long-term blood glucose levels within acceptable bounds. In addition, given the associated higher risks of cardiovascular disease, lifestyle modifications are recommended to control blood pressure.
Weight loss can prevent progression from prediabetes to diabetes type 2, decrease the risk of cardiovascular disease, or result in a partial remission in people with diabetes. No single dietary pattern is best for all people with diabetes. Healthy dietary patterns, such as the Merranean diet, low-carbohydrate diet, or DASH diet, are often recommended, although evidence does not support one over the others. According to the ADA, “reducing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia”, and for individuals with type 2 diabetes who cannot meet the glycemic targets or where reducing anti-glycemic medications is a priority, low or very-low carbohydrate diets are a viable approach. For overweight people with type 2 diabetes, any diet that achieves weight loss is effective.
A 2020 Cochrane systematic review compared several non-nutritive sweeteners to sugar, placebo and a nutritive low-calorie sweetener (tagatose), but the results were unclear for effects on HbA1c, body weight and adverse events. The studies included were mainly of very low-certainty and did not report on health-related quality of life, diabetes complications, all-cause mortality or socioeconomic effects.
Medications
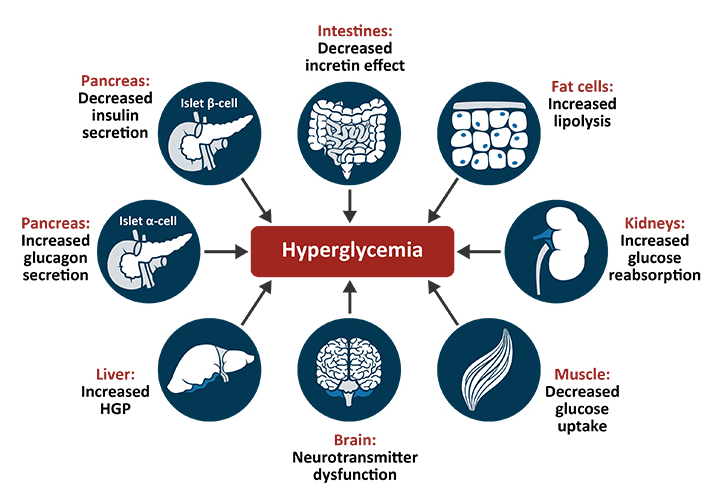
Glucose Control
Most medications used to treat diabetes act by lowering blood sugar levels through different mechanisms. There is broad consensus that when people with diabetes maintain tight glucose control – keeping the glucose levels in their blood within normal ranges – they experience fewer complications, such as kidney problems or eye problems. There is however debate as to whether this is appropriate and cost effective for people later in life in whom the risk of hypoglycemia may be more significant.
There are a number of different classes of anti-diabetic medications. Type 1 diabetes requires treatment with insulin, ideally using a “basal bolus” regimen that most closely matches normal insulin release: long-acting insulin for the basal rate and short-acting insulin with meals. Type 2 diabetes is generally treated with medication that is taken by mouth (e.g. metformin) although some eventually require injectable treatment with insulin or GLP-1 agonists.
Metformin is generally recommended as a first-line treatment for type 2 diabetes, as there is good evidence that it decreases mortality. It works by decreasing the liver’s production of glucose, and increasing the amount of glucose stored in peripheral tissue. Several other groups of drugs, mainly oral medication, may also decrease blood sugar in type 2 diabetes. These include agents that increase insulin release (sulfonylureas), agents that decrease absorption of sugar from the intestines (acarbose), agents that inhibit the enzyme dipeptidyl peptidase-4 (DPP-4) that inactivates incretins such as GLP-1 and GIP (sitagliptin), agents that make the body more sensitive to insulin (thiazolidinedione) and agents that increase the excretion of glucose in the urine (SGLT2 inhibitors). When insulin is used in type 2 diabetes, a long-acting formulation is usually added initially, while continuing oral medications.
Some severe cases of type 2 diabetes may also be treated with insulin, which is increased gradually until glucose targets are reached.
Blood Pressure Lowering
Cardiovascular disease is a serious complication associated with diabetes, and many international guidelines recommend blood pressure treatment targets that are lower than 140/90 mmHg for people with diabetes. However, there is only limited evidence regarding what the lower targets should be. A 2016 systematic review found potential harm to treating to targets lower than 140 mmHg, and a subsequent systematic review in 2019 found no evidence of additional benefit from blood pressure lowering to between 130 – 140mmHg, although there was an increased risk of adverse events.
2015 American Diabetes Association recommendations are that people with diabetes and albuminuria should receive an inhibitor of the renin-angiotensin system to reduce the risks of progression to end-stage renal disease, cardiovascular events, and death. There is some evidence that angiotensin converting enzyme inhibitors (ACEIs) are superior to other inhibitors of the renin-angiotensin system such as angiotensin receptor blockers (ARBs), or aliskiren in preventing cardiovascular disease. Although a more recent review found similar effects of ACEIs and ARBs on major cardiovascular and renal outcomes. There is no evidence that combining ACEIs and ARBs provides additional benefits.
Aspirin
The use of aspirin to prevent cardiovascular disease in diabetes is controversial. Aspirin is recommended by some in people at high risk of cardiovascular disease, however routine use of aspirin has not been found to improve outcomes in uncomplicated diabetes. 2015 American Diabetes Association recommendations for aspirin use (based on expert consensus or clinical experience) are that low-dose aspirin use is reasonable in adults with diabetes who are at intermediate risk of cardiovascular disease (10-year cardiovascular disease risk, 5–10%). National guidelines for England and Wales by the National Institute for Health and Care Excellence (NICE) recommend against the use of aspirin in people with type 1 or type 2 diabetes who do not have confirmed cardiovascular disease.
Surgery
Weight loss surgery in those with obesity and type 2 diabetes is often an effective measure. Many are able to maintain normal blood sugar levels with little or no medications following surgery and long-term mortality is decreased. There is, however, a short-term mortality risk of less than 1% from the surgery. The body mass index cutoffs for when surgery is appropriate are not yet clear. It is recommended that this option be considered in those who are unable to get both their weight and blood sugar under control.
A pancreas transplant is occasionally considered for people with type 1 diabetes who have severe complications of their disease, including end stage kidney disease requiring kidney transplantation.
Self-management and Support
In countries using a general practitioner system, such as the United Kingdom, care may take place mainly outside hospitals, with hospital-based specialist care used only in case of complications, difficult blood sugar control, or research projects. In other circumstances, general practitioners and specialists share care in a team approach. Evidence has shown that social prescribing led to slight improvements in blood sugar control for people with type 2 diabetes. Home telehealth support can be an effective management technique.
The use of technology to deliver educational programs for adults with type 2 diabetes includes computer-based self-management interventions to collect for tailored responses to facilitate self-management. There is no adequate evidence to support effects on cholesterol, blood pressure, behavioral change (such as physical activity levels and dietary), depression, weight and health-related quality of life, nor in other biological, cognitive or emotional outcomes.