Causes of Cancer
The GHS Hazard pictogram for carcinogenic substances Share of cancer deaths attributed to tobacco in 2016.
The majority of cancers, some 90–95% of cases, are due to genetic mutations from environmental and lifestyle factors. The remaining 5–10% are due to inherited genetics.
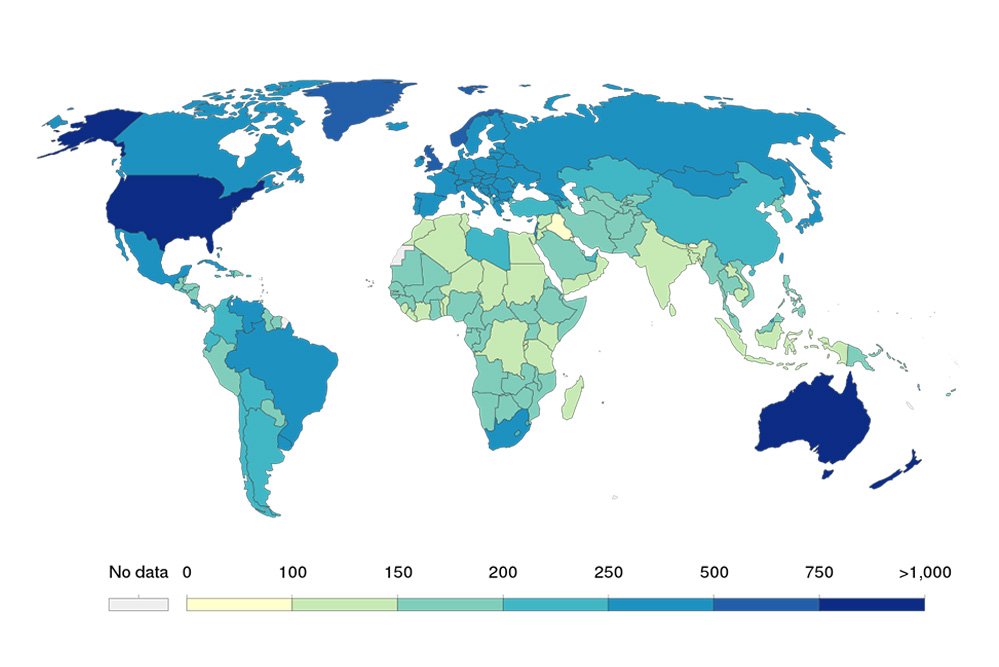
Environmental refers to any cause that is not inherited, such as lifestyle, economic, and behavioral factors and not merely pollution. Common environmental factors that contribute to cancer death include tobacco use (25–30%), diet and obesity (30–35%), infections (15–20%), radiation (both ionizing and non-ionizing, up to 10%), lack of physical activity, and pollution. Psychological stress does not appear to be a risk factor for the onset of cancer, though it may worsen outcomes in those who already have cancer.
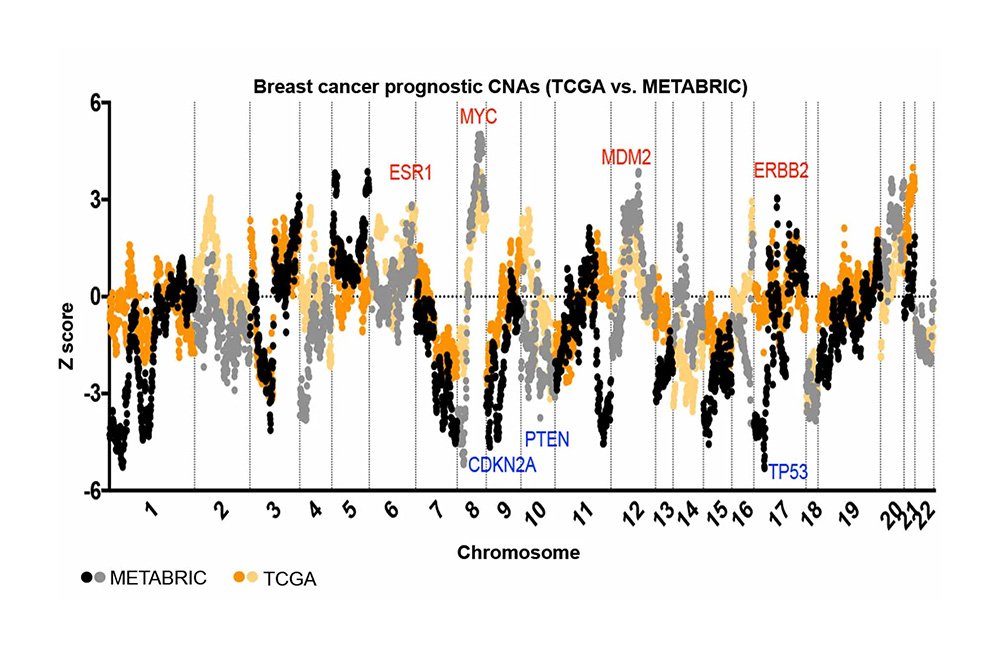
Environmental or lifestyle factors that caused cancer to develop in an individual can be identified by analyzing mutational signatures from genomic sequencing of tumor DNA. For example, this can reveal if lung cancer was caused by tobacco smoke, if skin cancer was caused by UV radiation, or if secondary cancers were caused by previous chemotherapy treatment.
Cancer is generally not a transmissible disease. Exceptions include rare transmissions that occur with pregnancies and occasional organ donors. However, transmissible infectious diseases such as hepatitis B, Epstein-Barr virus, Human Papilloma Virus and HIV, can contribute to the development of cancer.
Chemicals
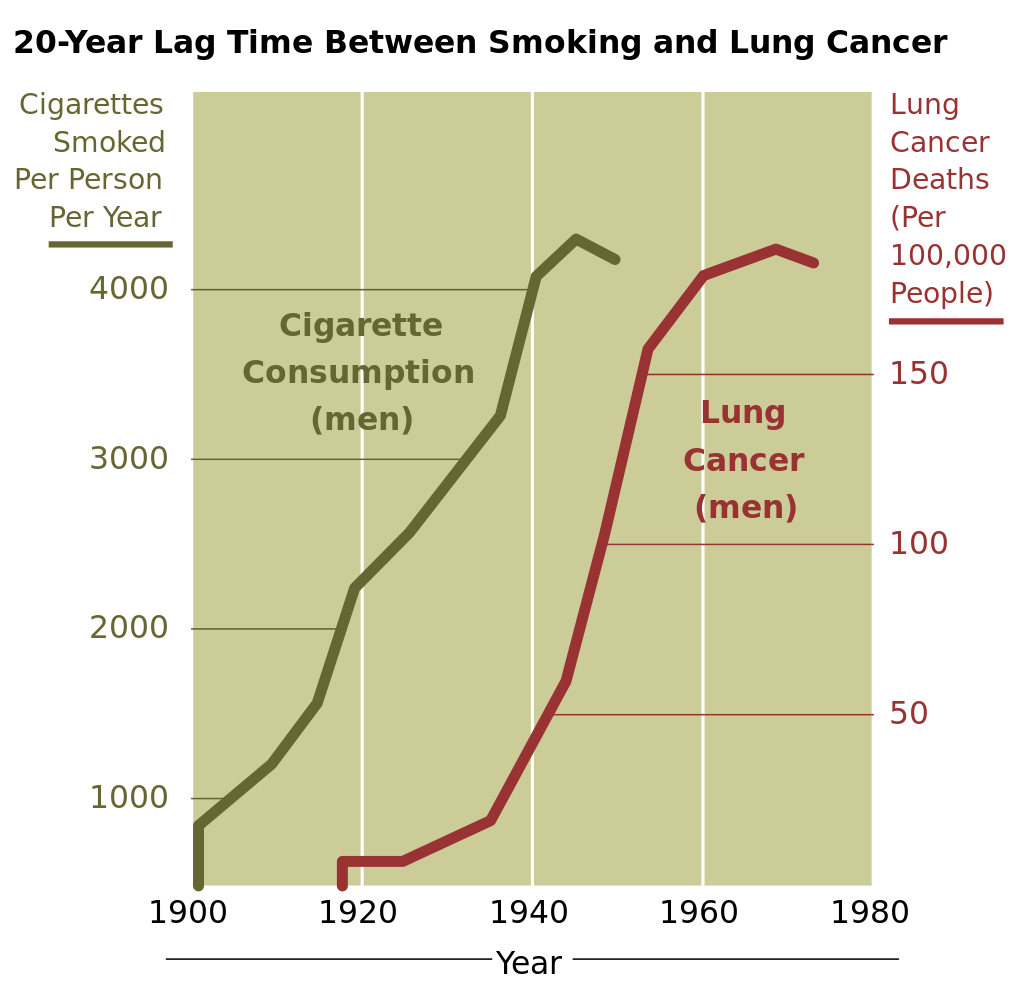
Further information: Alcohol and cancer and Smoking and cancer The incidence of lung cancer is highly correlated with smoking.
Exposure to particular substances have been linked to specific types of cancer. These substances are called carcinogens.
Tobacco smoke, for example, causes 90% of lung cancer. Tobacco use can cause cancer throughout the body including in the mouth and throat, larynx, esophagus, stomach, bladder, kidney, cervix, colon/rectum, liver and pancreas. Tobacco smoke contains over fifty known carcinogens, including nitrosamines and polycyclic aromatic hydrocarbons.
Tobacco is responsible for about one in five cancer deaths worldwide and about one in three in the developed world. Lung cancer death rates in the United States have mirrored smoking patterns, with increases in smoking followed by dramatic increases in lung cancer death rates and, more recently, decreases in smoking rates since the 1950s followed by decreases in lung cancer death rates in men since 1990.
In Western Europe, 10% of cancers in males and 3% of cancers in females are attributed to alcohol exposure, especially liver and digestive tract cancers. Cancer from work-related substance exposures may cause between 2 and 20% of cases, causing at least 200,000 deaths. Cancers such as lung cancer and mesothelioma can come from inhaling tobacco smoke or asbestos fibers, or leukemia from exposure to benzene.
Exposure to perfluorooctanoic acid (PFOA), which is predominantly used in the production of Teflon, is known to cause two kinds of cancer. Chemotherapy drugs such as platinum-based compounds are carcinogens that increase the risk of secondary cancers Azathioprine, an immunosuppressive medication, is a carcinogen that can cause primary tumors to develop.
Diet and exercise
Diet, physical inactivity, and obesity are related to up to 30–35% of cancer deaths. In the United States, excess body weight is associated with the development of many types of cancer and is a factor in 14–20% of cancer deaths. A UK study including data on over 5 million people showed higher body mass index to be related to at least 10 types of cancer and responsible for around 12,000 cases each year in that country.
Physical inactivity is believed to contribute to cancer risk, not only through its effect on body weight but also through negative effects on the immune system and endocrine system. More than half of the effect from the diet is due to overnutrition (eating too much), rather than from eating too few vegetables or other healthful foods. Some specific foods are linked to specific cancers. A high-salt diet is linked to gastric cancer. Aflatoxin B1, a frequent food contaminant, causes liver cancer. Betel nut chewing can cause oral cancer. National differences in dietary practices may partly explain differences in cancer incidence. For example, gastric cancer is more common in Japan due to its high-salt diet while colon cancer is more common in the United States. Immigrant cancer profiles mirror those of their new country, often within one generation.
Infection
Worldwide, approximately 18% of cancer deaths are related to infectious diseases. This proportion ranges from a high of 25% in Africa to less than 10% in the developed world. Viruses are the usual infectious agents that cause cancer but bacteria and parasites may also play a role. Oncoviruses (viruses that can cause human cancer) include:
- Human papillomavirus (cervical cancer),
- Epstein–Barr virus (B-cell lymphoproliferative disease and nasopharyngeal carcinoma),
- Kaposi’s sarcoma herpesvirus (Kaposi’s sarcoma and primary effusion lymphomas),
- Hepatitis B and hepatitis C viruses (hepatocellular carcinoma)
- Human T-cell leukemia virus-1 (T-cell leukemias).
- Merkel cell polyomavirus (Merkel cell carcinoma)
Bacterial infection may also increase the risk of cancer, as seen in
- Helicobacter pylori-induced gastric carcinoma.
- Colibactin, a genotoxin associated with Escherichia coli infection (colorectal cancer)
Parasitic infections associated with cancer include:
- Schistosoma haematobium (squamous cell carcinoma of the bladder)
- The liver flukes, Opisthorchis viverrini and Clonorchis sinensis (cholangiocarcinoma).
Radiation
Radiation exposure such as ultraviolet radiation and radioactive material is a risk factor for cancer. Many non-melanoma skin cancers are due to ultraviolet radiation, mostly from sunlight. Sources of ionizing radiation include medical imaging and radon gas. Ionizing radiation is not a particularly strong mutagen. Residential exposure to radon gas, for example, has similar cancer risks as passive smoking. Radiation is a more potent source of cancer when combined with other cancer-causing agents, such as radon plus tobacco smoke. Radiation can cause cancer in most parts of the body, in all animals and at any age. Children are twice as likely to develop radiation-induced leukemia as adults; radiation exposure before birth has ten times the effect.
Medical use of ionizing radiation is a small but growing source of radiation-induced cancers. Ionizing radiation may be used to treat other cancers, but this may, in some cases, induce a second form of cancer. It is also used in some kinds of medical imaging.
Prolonged exposure to ultraviolet radiation from the sun can lead to melanoma and other skin malignancies. Clear evidence establishes ultraviolet radiation, especially the non-ionizing medium wave UVB, as the cause of most non-melanoma skin cancers, which are the most common forms of cancer in the world.
Non-ionizing radio frequency radiation from mobile phones, electric power transmission and other similar sources has been described as a possible carcinogen by the World Health Organization’s International Agency for Research on Cancer. Evidence, however, has not supported a concern. This includes that studies have not found a consistent link between mobile phone radiation and cancer risk.
Heredity
The vast majority of cancers are non-hereditary (sporadic). Hereditary cancers are primarily caused by an inherited genetic defect. Less than 0.3% of the population are carriers of a genetic mutation that has a large effect on cancer risk and these cause less than 3–10% of cancer. Some of these syndromes include: certain inherited mutations in the genes BRCA1 and BRCA2 with a more than 75% risk of breast
cancer and ovarian cancer, and hereditary nonpolyposis colorectal cancer (HNPCC or Lynch syndrome), which is present in about 3% of people with colorectal cancer, among others.
Statistically for cancers causing most mortality, the relative risk of developing colorectal cancer when a first-degree relative (parent, sibling or child) has been diagnosed with it is about 2. The corresponding relative risk is 1.5 for lung cancer, and 1.9 for prostate cancer. For breast cancer, the relative risk is 1.8 with a first-degree relative having developed it at 50 years of age or older, and 3.3 when the relative developed it when being younger than 50 years of age.
Taller people have an increased risk of cancer because they have more cells than shorter people. Since height is genetically determined to a large extent, taller people have a heritable increase of cancer risk.
Physical agents
Some substances cause cancer primarily through their physical, rather than chemical, effects. A prominent example of this is prolonged exposure to asbestos, naturally occurring mineral fibers that are a major cause of mesothelioma (cancer of the serous membrane) usually the serous membrane surrounding the lungs. Other substances in this category, including both naturally occurring and synthetic asbestos-like fibers, such as wollastonite, attapulgite, glass wool and rock wool, are believed to have similar effects. Non-fibrous particulate materials that cause cancer include powdered metallic cobalt and nickel and crystalline silica (quartz, cristobalite and tridymite). Usually, physical carcinogens must get inside the body (such as through inhalation) and require years of exposure to produce cancer.
Physical trauma resulting in cancer is relatively rare. Claims that breaking bones resulted in bone cancer, for example, have not been proven. Similarly, physical trauma is not accepted as a cause for cervical cancer, breast cancer or brain cancer. One accepted source is frequent, long-term application of hot objects to the body. It is possible that repeated burns on the same part of the body, such as those produced by kanger and kairo heaters (charcoal hand warmers), may produce skin cancer, especially if carcinogenic chemicals are also present. Frequent consumption of scalding hot tea may produce esophageal cancer. Generally, it is believed that cancer arises, or a pre-existing cancer is encouraged, during the process of healing, rather than directly by the trauma. However, repeated injuries to the same tissues might promote excessive cell proliferation, which could then increase the odds of a cancerous mutation.
Chronic inflammation has been hypothesized to directly cause mutation. Inflammation can contribute to proliferation, survival, angiogenesis and migration of cancer cells by influencing the tumor microenvironment. Oncogenes build up an inflammatory pro-tumorigenic microenvironment.
Hormones
Hormones also play a role in the development of cancer by promoting cell proliferation. Insulin-like growth factors and their binding proteins play a key role in cancer cell proliferation, differentiation and apoptosis, suggesting possible involvement in carcinogenesis.
Hormones are important agents in sex-related cancers, such as cancer of the breast, endometrium, prostate, ovary and testis and also of thyroid cancer and bone cancer. For example, the daughters of women who have breast cancer have significantly higher levels of estrogen and progesterone than the daughters of women without breast cancer. These higher hormone levels may explain their higher risk of breast cancer, even in the absence of a breast-cancer gene. Similarly, men of African ancestry have significantly higher levels of testosterone than men of European ancestry and have a correspondingly higher level of prostate cancer. Men of Asian ancestry, with the lowest levels of testosterone-activating androstanediol glucuronide, have the lowest levels of prostate cancer.
Other factors are relevant: obese people have higher levels of some hormones associated with cancer and a higher rate of those cancers. Women who take hormone replacement therapy have a higher risk of developing cancers associated with those hormones. On the other hand, people who exercise far more than average have lower levels of these hormones and lower risk of cancer. Osteosarcoma may be promoted by growth hormones. Some treatments and prevention approaches leverage this cause by artificially reducing hormone levels and thus discouraging hormone-sensitive cancers.
Autoimmune diseases
There is an association between celiac disease and an increased risk of all cancers. People with untreated celiac disease have a higher risk, but this risk decreases with time after diagnosis and strict treatment. This may be due to the adoption of a gluten-free diet, which seems to have a protective role against development of malignancy in people with celiac disease. However, the delay in diagnosis and initiation
of a gluten-free diet seems to increase the risk of malignancies. Rates of gastrointestinal cancers are increased in people with Crohn’s disease and ulcerative colitis, due to chronic inflammation. Immunomodulators and biologic agents used to treat these diseases may promote developing extra-intestinal malignancies.