Diabetes Society and Culture
The 1989 “St. Vincent Declaration” was the result of international efforts to improve the care accorded to those with diabetes. Doing so is important not only in terms of quality of life and life expectancy but also economically – expenses due to diabetes have been shown to be a major drain on health – and productivity-related resources for healthcare systems and governments.
Several countries established more and less successful national diabetes programmes to improve treatment of the disease
Diabetes Stigma
Diabetes stigma describes the negative attitudes, judgment, discrimination, or prejudice against people with diabetes. Often, the stigma stems from the idea that diabetes (particularly Type 2 diabetes) resulted from poor lifestyle and unhealthy food choices rather than other causal factors like genetics and social determinants of health. Manifestation of stigma can be seen throughout different cultures and contexts. Scenarios include diabetes statuses affecting marriage proposals, workplace-employment, and social standing in communities.
Stigma is also seen internally, as people with diabetes can also have negative beliefs about themselves. Often these cases of self-stigma are associated with higher diabetes-specific distress, lower self-efficacy, and poorer provider-patient interactions during diabetes care.
Racial and Economic Inequalities
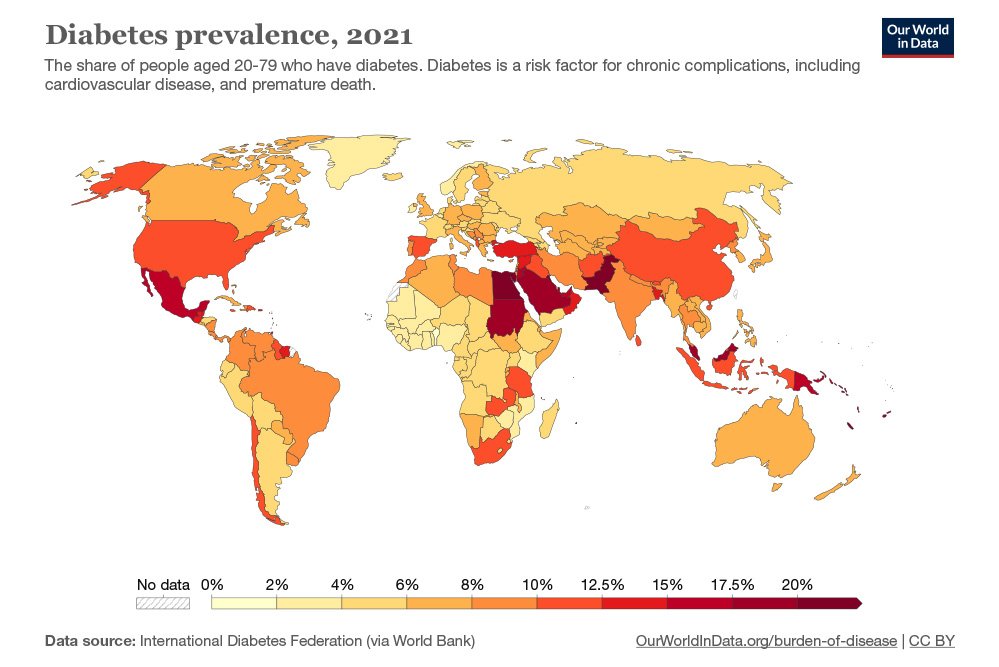
Racial and ethnic minorities are disproportionately affected with higher prevalence of diabetes compared to non-minority individuals. While US adults overall have a 40% chance of developing type 2 diabetes, Hispanic/Latino adults chance is more than 50%. African Americans also are much more likely to be diagnosed with diabetes compared to White Americans. Asians have increased risk of diabetes as diabetes can develop at lower BMI due to differences in visceral fat compared to other races. For Asians, diabetes can develop at a younger age and lower body fat compared to other groups. Additionally, diabetes is highly underreported in Asian American people, as 1 in 3 cases are diagnosed compared to the average 1 in 5 for the nation.
People with diabetes who have neuropathic symptoms such as numbness or tingling in feet or hands are twice as likely to be unemployed as those without the symptoms.
In 2010, diabetes-related emergency room (ER) visit rates in the United States were higher among people from the lowest income communities (526 per 10,000 population) than from the highest income communities (236 per 10,000 population). Approximately 9.4% of diabetes-related ER visits were for the uninsured.
Naming
The term “type 1 diabetes” has replaced several former terms, including childhood-onset diabetes, juvenile diabetes, and insulin-dependent diabetes mellitus. Likewise, the term “type 2 diabetes” has replaced several former terms, including adult-onset diabetes, obesity-related diabetes, and noninsulin-dependent diabetes mellitus. Beyond these two types, there is no agreed-upon standard nomenclature.
Diabetes mellitus is also occasionally known as “sugar diabetes” to differentiate it from diabetes insipidus.